News review – March 2020
 At Westminster, the new Parliament began to move into gear. Aside from the resignation of chancellor Sajid Javid – who was replaced by his deputy, Rishi Sunak – just weeks before the 11 March Budget, a familiar face came back into health politics. Former health secretary Jeremy Hunt was confirmed as the new chair of the Commons Health and Social Care committee. Meanwhile, Meg Hillier was re-elected chair of the Commons Public Accounts Committee.
At Westminster, the new Parliament began to move into gear. Aside from the resignation of chancellor Sajid Javid – who was replaced by his deputy, Rishi Sunak – just weeks before the 11 March Budget, a familiar face came back into health politics. Former health secretary Jeremy Hunt was confirmed as the new chair of the Commons Health and Social Care committee. Meanwhile, Meg Hillier was re-elected chair of the Commons Public Accounts Committee.
Getting health and social care staffing levels right will be crucial to the delivery of the NHS long-term plan, and NHS England and NHS Improvement will outline their strategy in the NHS People Plan, due in March or April. However, the government’s announcement of its plans for a new points-based immigration system in February caused consternation. Although the system will make special allowances for the recruitment of NHS staff, there is no provision for social care workers. According to the Health Foundation, 17% of adult social care staff are non-British nationals, while in London the figure is closer to 40%. The King’s Fund praised the recognition of the need for overseas workers in the NHS, but added there are more than 120,000 vacancies in social care. Many people were struggling to access the support needed to live independently and avoid long stays in hospital.
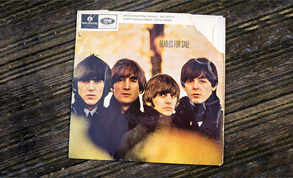 The NHS in England needs the biggest rebuilding programme since The Beatles were in their pomp, according to NHS Providers. While recent capital funding announcements are welcome, they fall well short of what is required. In a new report, Rebuilding our NHS: why it’s time to invest, the providers body said that in a survey of NHS leaders, 97% were worried that their organisation’s capital needs would not be met. The last, and only, major national hospital building programme was in the 1960s, which delivered 95 schemes in its first three years. The government has, so far, announced 40 projects – showing more modest ambition than previous initiatives, NHS Providers said.
The NHS in England needs the biggest rebuilding programme since The Beatles were in their pomp, according to NHS Providers. While recent capital funding announcements are welcome, they fall well short of what is required. In a new report, Rebuilding our NHS: why it’s time to invest, the providers body said that in a survey of NHS leaders, 97% were worried that their organisation’s capital needs would not be met. The last, and only, major national hospital building programme was in the 1960s, which delivered 95 schemes in its first three years. The government has, so far, announced 40 projects – showing more modest ambition than previous initiatives, NHS Providers said.
 A two-year delay in breaking ground on a building project can add 36% to the cost, according to health and care property development company Prime. In its report, Ending change paralysis in NHS estates: how to forge ahead in uncertain times, the company said a three-year delay can increase costs to ‘an incredible, often insurmountable, 49%’. It argued that NHS organisations must create their own momentum to deliver projects sooner, or risk their plans being derailed as costs rise.
A two-year delay in breaking ground on a building project can add 36% to the cost, according to health and care property development company Prime. In its report, Ending change paralysis in NHS estates: how to forge ahead in uncertain times, the company said a three-year delay can increase costs to ‘an incredible, often insurmountable, 49%’. It argued that NHS organisations must create their own momentum to deliver projects sooner, or risk their plans being derailed as costs rise.
The Institute for Public Policy Research (IPPR) urged the government to invest in the primary care estate by allocating £500m a year for a decade to build 1,300 new primary care hubs. The IPPR report, Realising the neighbourhood NHS: delivering a new deal for primary care, also called for the traditional GP partnership model to be phased out. Rather than being independent contractors, GPs should be salaried. This would allow them to focus on patients, rather than managing a business – improving quality and access to care, and addressing workforce shortages.
With some commissioners forecasting an underspend on additional roles funding in 2019/20, NHS England encouraged primary care networks (PCNs) to recruit now to any of the 10 roles included in the scheme from April. Funding for the new roles is included in the new GP contract, agreed between the government and the British Medical Association. There will also be funding for recruitment and retention schemes to deliver 6,000 extra GPs; a renewed focus on improving access; moves to improve vaccination coverage; and an investment and impact fund to reward PCNs that deliver their objectives. The investment fund will be worth £40.5m in 2020/21, rising to £150m in 2021/22, £225m in 2022/23 and £300m in 2023/24.
According to NHS Resolution, a total of 117 trusts achieved all 10 safety actions in the second year of the maternity incentive scheme. The scheme was set up at the end of 2017 to incentivise improved maternity safety. Trusts that achieve all 10 actions recover their contribution to the maternity incentive fund (an additional 10% of the Clinical Negligence Scheme for Trusts maternity premium) and share in any unallocated funds. Maternity claims account for 60% of the annual £9bn cost of harm under the CNST. Details of year three of the scheme have also been published.
NHS Employers has not included specific recommendations in its evidence to the Doctors’ and Dentists’ Pay Review Body (DDRB) for 2020/21. The organisation said junior doctors have a multi-year deal, while any pay increase for specialist and associate specialist (SAS) doctors is likely to be linked to contract reform. Employing bodies have told NHS Employers that they are not in favour of targeting pay at specific specialties or localities.
The NHS invested more than 50% of the apprenticeship levy (£200m) back into apprenticeships in 2019/20, representing a significant improvement on the previous year. NHS England and NHS Improvement urged every trust to aim for 100% in 2020/21. NHS employers were asked recently to review workforce plans to ensure that they make full use of the apprenticeship levy. Chief nursing officer Ruth May insisted that the NHS must increase its nurse apprenticeships if it is to deliver the ambitions of the NHS long-term plan. Almost 1,800 nurse apprentices started their courses over the last two years, but the NHS requires thousands more. Boosting apprenticeships is part of the government’s plan to increase recruitment and retention.
The month in quotes
‘The NHS is providing world-class care for more patients than ever, and to carry on doing that we need 50,000 more nurses. Boosting the number of nursing apprentices is one important way we can achieve that goal, and as we deliver on our NHS long-term plan we want local health service employers to ramp up the opportunities they offer in their areas.’
Ruth May, chief nursing officer for England, calls for more nursing apprenticeships
‘It’s time for the biggest building programme in the NHS since The Beatles. This will support delivery of the long-term plan and provide the opportunity to see tangible improvements to patient safety and staff and patient experience.’
NHS Providers deputy chief executive Saffron Cordery
 ‘Over nearly a decade in frontline politics, the NHS has always been my greatest political passion, and I am honoured to have been elected chair of the Health and Social Care Select Committee. I look forward to working with my committee to provide a strong, independent voice that supports health and social care services in a very pressured period.’
‘Over nearly a decade in frontline politics, the NHS has always been my greatest political passion, and I am honoured to have been elected chair of the Health and Social Care Select Committee. I look forward to working with my committee to provide a strong, independent voice that supports health and social care services in a very pressured period.’
Former health secretary Jeremy Hunt on his return to the health arena
 ‘While it’s positive the government recognises the need for overseas workers to help plug gaps in the NHS workforce, there is a disappointing lack of consideration given to social care. The NHS workforce is only half the story.’
‘While it’s positive the government recognises the need for overseas workers to help plug gaps in the NHS workforce, there is a disappointing lack of consideration given to social care. The NHS workforce is only half the story.’
King’s Fund director of leadership and organisational development Suzie Bailey
From the HFMA
Collecting patient-relevant outcomes is not just about comparing performance or to inform payments, but also to ensure that patient needs are understood, communication between patient and clinician is enhanced, and to support new models of care. So says GP Sally Lewis, NHS Wales’ national clinical director for value-based healthcare, in a blog for the HFMA. Dr Lewis says achieving value is about delivering the outcomes patients want within available resources. Although collecting, analysing and using patient data at scale can be a major undertaking, she believes the benefits mean finance directors will support investment in it.
Value-based healthcare is also the subject of a blog from Healthcare Costing for Value Institute head Catherine Mitchell. She focuses on a new framework that aims to help clinicians and finance professionals work together to implement value-based healthcare. Clinicians must better understand costing if the NHS is to harness patient-level data to improve services and patient outcomes, she argues. The Engagement Value Outcome framework developed by the institute and Future-Focused Finance aims to help overcome this, bringing together clinicians, operational managers, and finance and informatics staff.
HFMA policy and research manager Lisa Robertson blogs about issues facing non-executive directors and lay members in the annual report and accounts process. Non-execs have a key role in ensuring the annual report and accounts reflect their organisation’s position. And, as year-end approaches, it is a good time to ensure they are up to date with the latest guidance, she says.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.