News / News review - February 2017
While stories of an NHS in disarray dominated many news bulletins in early January, we learnt in the previous month that local authorities would be given greater flexibility to raise funding for social care. Lack of resources in social care is believed to be one of the chief contributing factors to the climbing attendances at A&E – which in turn increases waiting times – and delayed transfers of care of patients well enough to be discharged from hospital but who do not have a package of care in the community.
In mid-December, communities and local government secretary Sajid Javid said social care would get extra funding in the next two financial years. Changes to the council tax precept for social care and savings from reform of the new homes bonus could boost social care spending by almost £900m by 2019, he said. The social care precept can now be raised by 3% rather than the current 2%, providing a potential additional £208m in 2017/18 and £444m in 2018/19. The new homes savings would amount to £240m. But he warned that variations in social care must be tackled and it was ‘vital that we finish the job of integrating our health and social care systems’. And NHS Providers warned there were limitations on the new money. It said that while councils would have the freedom to increase the precept by up to 3% in the next two years, they would be unable to raise it by more than 6% over the three-year period set by the original precept conditions.
Meanwhile, NHS Providers reported that cuts in community beds and other services are hampering acute trusts’ attempts to cope with rising demand. In its survey, Delivering care in every setting, more than half (52%) of chief executives, chief operating officers and finance directors who responded said it had become more difficult to deal with demand for community-based services over the last two years. Despite the direction set by the Five-year forward view, they said there were significant reductions in community beds because of lack of funding, staff shortages and a reduction in capacity.
The Scottish government is also pressing for greater health and social care integration, saying it will invest an additional £107m in the next financial year. It said the funding would ensure people were cared for safely in their own homes and would help avoid unnecessary hospital admissions. As outlined in the government’s draft Budget, the £107m will transfer from the NHS to health and social care partnerships in 2017/18. It is in addition to the £250m added in the current financial year, which will be part of the baseline from 2017/18.
In Wales, health secretary Vaughan Gething (right) announced a £31m funding package to improve neonatal and obstetric services in two hospitals. More than £25m will be invested in redeveloping the neonatal and obstetric services at the University Hospital of Wales. This will include additional beds and a dedicated obstetric operating theatre. And £6m will be spent consolidating and redeveloping services at Prince Charles Hospital, Cwm Taf, with extra neonatal beds and maternity facilities. 
Staying in the principality, employers in Wales have reiterated their commitment to improving medical engagement. The pledge followed publication of a survey that showed engagement was patchy in NHS bodies across the country. For the first time, doctors were invited to take part in the survey – known as the medical engagement scale – which revealed some examples of good engagement and others where significant improvement was needed. A joint statement from the Welsh NHS Confederation and BMA Cymru Wales said improving medical engagement was a priority. The bodies will work together to achieve this over the next three years, when the survey will be repeated.
The NHS Confederation has appointed
Niall Dickson (right) as its new chief executive. Mr Dickson, a former BBC social affairs editor and chief executive of the King’s Fund and the General Medical Council, will join the confederation on 1 February. 
Barcoding of patients, medical supplies and equipment has the potential to save lives and up to £1bn over seven years, the Department of Health said. Highlighting initial findings from its £12m Scan4Safety project, it said barcodes were helping track patients and their treatment. Faulty equipment could be traced and patients identified, even if the fault came to light years later, it said. Early results from six pilots showed lives and money would be saved through reducing waste, the Department added.
NHS Improvement has been asked to prioritise an increase in the average tenure of NHS provider chief executives. In a remit letter to the oversight body, health minister Philip Dunne set out NHS Improvement’s objectives for the current year and the rest of the Parliament. NHS Improvement must also strengthen the pipeline of chief executive, finance director and chief operating officer applicants through proven talent management approaches and succession planning. The organisation announced a new aspiring leaders’ talent pool at the HFMA annual conference in December. The remit sets objective in five areas:
- Budget
- High-quality care
- Operational performance
- Five-year forward view
- Leadership.
It sets out NHS Improvement’s role in supporting the roll-out of seven-day service standards and delivering improved patient-level costing.
Just over £100m in new funding has been allocated by NHS England to support and spread the work of the new care model vanguards. In addition, the vanguards will continue to receive support from NHS England and other national bodies to implement their plans, including how they harness new technology such as apps and shared computer systems. They are also receiving help to develop their workforce so that it is organised around patients and their local populations. The total funding allocated equals that of 2016/17 and will be matched by funds and resources from the vanguards themselves.
In the media
December and January were busy months for the HFMA, with the publication of the latest NHS financial temperature check, the annual conference, the launch of the new qualifications and the winter pressures faced by the NHS. 
The latter led to an appearance on BBC
Radio 5 Live’s Wake up to money by
HFMA policy director Paul Briddock (right). He said the NHS financial position had been deteriorating for two to three years. He explained how the estimated £30bn gap in NHS funding would be bridged, with an extra £8bn in funding and £22bn in efficiency savings. Asked if NHS managers should be doing more to deliver services within budget, he said the service had been asked to achieve relatively high levels of efficiency since 2010 – historically such levels had not been sustained in the NHS or in other healthcare systems.
The temperature check attracted a lot of media attention, including Onmedica, a website for health professionals. Mr Briddock said finance directors were initially enthusiastic about sustainability and transformation plans (STPs), but the temperature check showed scepticism that they can work.
Health Service Journal reported on NHS Improvement chief executive Jim Mackey telling the annual conference that finance directors should not bow to pressure to hide the true financial position. And, in January, Public Finance published an article from Mr Briddock outlining the need for all staff to understand finance and introducing the new HFMA qualifications.
Quotes
‘Knowledge is power. Not only does this provide us with a level of data and insight to better challenge clinical practice and variation, it helps to safeguard our patients from avoidable harm. In the event of a product recall, we can easily track an affected product to the right patient.’ 
Tim Wells, consultant cardiologist at Salisbury NHS Foundation Trust, on the Scan4Safety barcoding
‘2017/18 is a crucial year for the vanguards, in particular how we further spread their work across the wider NHS and care services. This funding, as well as the support we offer to them, will help them to continue to move at pace.’
Samantha Jones, director of the new care models programme at NHS England, says vanguards are developing quickly, helped by new funding
‘It is vital we finish the job of integrating our health and social care systems. We know this can improve outcomes and make funding go further, helping people manage their health and wellbeing and to live independently for as long as possible.’
Sajid Javid (right) says new social care funding must be accompanied by reform 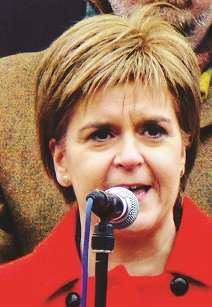
‘Not only does it ensure patients can
receive more treatment in their communities but it also reduces demand for acute hospital usage by reducing avoidable admissions, lengths of stay and delayed discharges.’
Scottish first minister Nicola Sturgeon (right) on why her government has committed a further £107m for health and social care integration
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.