Revised finance framework revealed
At a joint board meeting earlier this week, the national bodies said the updated framework would likely begin in October and retain many of the features of the temporary finance regime in operation since April. This system is based on block contracts with prospective and retrospective top-ups to cover additional Covid costs.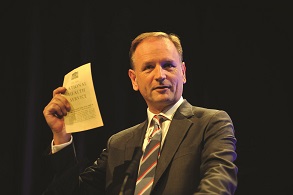
A letter issued by NHS England chief executive Simon Stevens (pictured) and NHS chief operating officer Amanda Pritchard this afternoon gave more details. It confirmed commissioners and providers will continue to use nationally calculated block contracts, together with a greater emphasis on system finance and incentives for restoring elective services. (The HFMA has produced a summary of the key points in the letter.)
The revised financial framework will see a return to ‘the usual financial disciplines’. Once implemented, there will no longer be retrospective top-up payments and providers and commissioners will be expected to achieve balance within their financial envelopes. However, while systems must break even overall, individual trusts and clinical commissioning groups will be allowed to deliver mutually agreed surpluses or deficits.
The new funding envelope will have four parts:
- CCG allocations – the value of block contracts for NHS providers will continue to be nationally calculated
- Directly commissioned services from NHS providers – the value of these contracts will also be calculated nationally
- Top-up – additional funding provided to support the delivery of a breakeven position
- Non-recurrent Covid allocation – this is additional funding to cover Covid-related costs for the remainder of the financial year.
While nationally calculated block contracts will continue to be used, payments will be adjusted according to delivery against activity restart goals, which are also set out in the letter. The restart goals, known as A1 and A2, include the full restoration of all cancer services (A1). This means ensuring referrals return to at least pre-pandemic levels and managing the growth in cancer diagnosis and treatment.
The A2 goal focuses on recovering the maximum level of elective activity possible before winter. Trusts and systems are expected to re-establish – and, where necessary, redesign – local NHS services. It sets clear targets – in September, they should deliver at least 80% of last year’s activity for overnight and outpatient/day case elective procedures. They should aim for 70% in August and increase the figure to 90% in October.
To support these activity levels, providers must quickly return to at least 90% of last year’s MRI, CT and endoscopy procedures, and aim for 100% by October. First outpatient attendances and follow-ups – face-to-face or virtually – should be at 100% of 2019/20 activity from September (aiming for 90% in August).
Block payments for low-volume CCG-commissioned activity will be made via the provider’s host CCG, removing the need for separate invoicing of non-contract activity.
Written contracts between commissioners and providers for the remainder of 2020/21 will not be required.
Adjustments to published commissioner allocations will continue and will take account of changes in contracting responsibility and distribution of the top-up to CCGs within the local system, based on target allocation.
Reimbursement for high-cost drugs under the Cancer Drugs Fund and relating to the hepatitis C programme will revert to payment under a pass-through cost and volume basis. NHS provider block contracts will be adjusted to reflect this.
For most other high-cost drugs and devices, the national bodies will track the in-year provider spend against a notional level of spend included in the block payments. Adjustments will be made in-year to ensure providers are reimbursed for their actual expenditure. NHS England and NHS Improvement said this would leave a smaller list of high-cost drugs that will still be funded under the block arrangements.
The letter also includes information on meeting the costs of medical pay awards announced in July. The national bodies expect the rises to be implemented in September salaries, backdated to April. Providers should claim for additional costs in September as part of the retrospective top-up process. Future costs will be taken into account for the rest of 2020/21, and further details are expected in due course.
NHS Providers chief executive Chris Hopson said the activity targets ‘look very stretching’. Though there was a lot to do to recover services, it was ‘important that we are ambitious for patients’. He added providers were nervous about the reintroduction of continuing healthcare assessments and warned work on freeing up bed capacity could be undone if there are disagreements over who funds packages long term.
He continued: ‘The letter provides a new financial framework for trusts. But we can’t really judge the approach until we know what the financial envelope is for the second half of the year and how that translates into individual allocations for organisations. That’s still being negotiated with the Treasury and probably won’t be finalised for at least another month.
‘The renewed commitment to system working and collaboration is also welcomed by trusts but, longer term, we need much greater clarity on accountabilities and governance if revenue funding is to be allocated to systems that currently have no statutory underpinning and no formal accounting officer status.’
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.