NHS in numbers: lifestyle factors
 A new review led by Michael Marmot - Health equity in England: the Marmot review 10 years on –reports that life expectancy has stalled since 1990, with growing differences between the most and least deprived areas. Healthy life expectancy has declined for women over the same time period and the percentage of life spent in ill health has increased for men and women.
A new review led by Michael Marmot - Health equity in England: the Marmot review 10 years on –reports that life expectancy has stalled since 1990, with growing differences between the most and least deprived areas. Healthy life expectancy has declined for women over the same time period and the percentage of life spent in ill health has increased for men and women.
The Health profile for England: 2019 also shows a small increase in the age standardised morbidity rate since 1990, although the previous year’s data, using a slightly different methodology had shown a slight decrease. The profile backs up Marmot’s figures on healthy life expectancy, although the changes are very small.
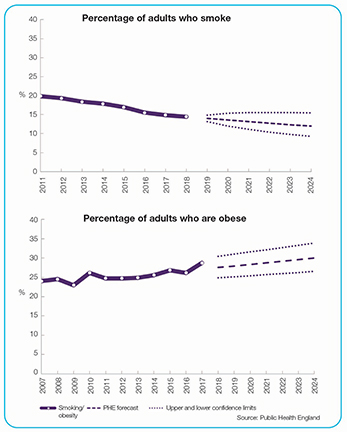
Smoking and obesity are among the leading risk factors for morbidity, associated with cardiovascular disease, musculoskeletal conditions, respiratory diseases, diabetes and most cancers.
The prevalence of smoking has continued to decline over the last seven years to 14.4% of adults (18+) in 2018. A time series analysis suggests that if this trend continues, it will reduce to between 8.5% and 11.7% by 2023. Office for National Statistics figures show that rates are higher in the other UK nations, with rates rising from Northern Ireland (15.5%), through Wales (15.9%) to Scotland (16.3%). The rate across the whole UK is 14.7%.
Figures from the OECD, show that UK smoking rates are below the OECD average. The OECD’s Health at a glance 2019 publication uses figures that are not directly comparable to the ONS figures – they use a different survey source and define adults as 15+. It puts the UK smoking rate for 2017 at 17.2%, compared with an OECD average of 18%. Rates range from 25% in Greece, Turkey, Hungary and France to below 10% in Mexico and Iceland.
The NHS long-term plan says that, while rates have fallen, smoking still accounts for more years of life lost than any modifiable risk factor. Around 6.1 million people in England still smoke. Smokers see their GP over a third more often than non-smokers and smoking is linked to nearly half a million hospital admissions each year, costing more than £900m.
Add in the cost of primary and ambulatory care services and the cost rises to £2.4bn, according to pressure group Ash’s 2019 costs of tobacco ready reckoner. The cost of smoking-related social care is nearly £900m and the total cost to society each year is estimated to be £12.5bn, when you add in lost productivity.
Smoking cessation services are commissioned by local authorities. However, according to the long-term plan, all patients admitted to hospital will be offered NHS-funded tobacco treatment services by 2023/24.
NHS Digital statistics show that in 2017/18, 10,660 hospital admissions were directly attributable to obesity (primary diagnosis) and there were 711,000 admissions where obesity was a factor (primary or secondary diagnosis). The latter is an increase of 15% on 2016/17, although some of this may be due to better recording. For admissions where obesity was a factor, there were a large number of different primary diagnoses. Less than a quarter of all of them related to the top ten diagnosis types – although the most common related to joint issues and maternity issues.
Alcohol misuse is the biggest risk factor attributable to early mortality, ill-health and disability for people aged 15 to 49 (and is the fifth most important for all ages). According to NHS Digital statistics (2019), some 21% of adults (16+) drink more than 14 units per week. There were 338,000 hospital admissions in 2017/18, where the main reason for admission was attributable to alcohol. This is 15% higher than 2007/08 and represents 2.1% of all hospital admissions.
Blackpool had the highest rate at 1,100 per 100,000 population, Wokingham had the lowest rate at 390.
There were 1.2 million admissions where the primary reason for hospital admission or a secondary diagnosis was linked to alcohol – representing 7.2% of all hospital admissions.
Related content
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.
This webinar series offers colleagues of ICS organisations the opportunity to discuss common priorities, challenges, and successes within their field.