HFMA 2020: NHS has role in addressing wider determinants of health
Jo Bibby, (pictured on screen) director of health at the Health Foundation, argued that there were signs of increasing health inequalities related to income, employment and housing. There has been a slowing down in improvements in life expectancy, with life expectancy even starting to fall for some groups. And there were clear links between life expectancy and healthy life expectancy and a person’s wealth.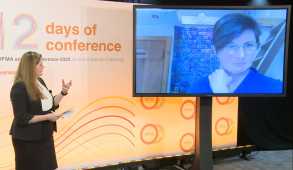
‘The Covid-19 pandemic has really illuminated and amplified a lot of the issues,’ she told delegates.
She detailed increasing evidence showing the impact that socio-economic factors can have on health. ‘But there is less evidence on what difference good health makes to our society – as individuals and collectively,’ she said. ‘And this year has shown us that if we are not a nation with good health, it begins to impact on our ability to function as a society.’
While this may have been in unique circumstances, the same patterns could be seen with the more usual diseases and conditions that people present with. ‘These illnesses do affect the ability for people to participate effectively in society,’ she said.
The foundation is undertaking some econometric analysis to look at the value that good health contributes to society. Ms Bibby said that early results show that poor mental health does affect people’s ability to contribute to the economy. And childhood obesity impacts on attainment, which flows through to an ability to participate in work.
‘We are interested in putting a value on the contribution that good health makes because this starts to build a better case for some of the arguments for investment in the areas that keep people in good health in the first place and prevent deterioration,’ she said.
Many of these areas are out of the direct control of NHS, and while NHS budgets have seen some form of year-on-year increases in recent years, other spending areas have been subject to significant cuts. But the NHS did have a part to play, Ms Bibby said.
First it could do more on prevention. For example, there is inequality in access with people from more deprived areas more likely to have a cancer diagnosis in accident and emergency rather than earlier on in general practice. ‘Do we know enough about where the prevention spend is going in the NHS? Is it enough, is it the right balance? These are all questions that the finance profession could be thinking about,’ she said.
Other health systems were paying more attention to living conditions. ‘What is the point of treating people, only to send them back to the conditions that are making them ill,’ she asked.
The second area where the NHS could get involved is as anchor institutions. This could involve thinking more about procuring locally, making buildings available for local use and ensuring employment also provides opportunities for people living in more disadvantaged areas.
And finally, she said the NHS should be doing more as a system partner. She highlighted a new health index from the Office for National Statistics that provides a GDP-like measure of how an area is doing on health. It draws on three domains including: healthy people, healthy lives and healthy places. ‘This tool creates some good opportunities to have good conversations locally,’ she said.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.