Convergence reduces over-target ICB allocations
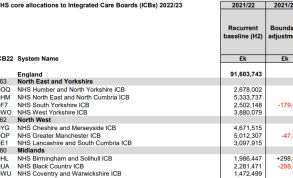 Technical guidance on ICB allocations sets out how almost £95bn has been allocated to local systems. It introduced the principle of convergence, which replaces pace of change as a method of moving systems’ budgets closer to target. The convergence requirement ensures the distribution of funding does not exceed the available budget as set out in the 2021 spending review, and moves ICBs towards fair share allocations. Systems consuming more than their fair share will have a greater convergence requirement.
Technical guidance on ICB allocations sets out how almost £95bn has been allocated to local systems. It introduced the principle of convergence, which replaces pace of change as a method of moving systems’ budgets closer to target. The convergence requirement ensures the distribution of funding does not exceed the available budget as set out in the 2021 spending review, and moves ICBs towards fair share allocations. Systems consuming more than their fair share will have a greater convergence requirement.
Before applying the convergence factor, average core services growth in 2022/23 is estimated at 4%, and 6.5% for primary medical services. While the latter remains the same after convergence, the former is reduced to 3.6% average growth.
As with pace of change policy in previous years, applying the convergence factor means that ICBs furthest above target receive less growth. Those below target receive more. The approach ensures stability – setting growth for under target systems at levels that can be deployed effectively, while not undermining financial confidence in over-target ICBs.
Only four ICBs remain under target in 2022/23.
For core services, ICBs that are 1% or more below target receive an additional 0.25%. For those between 1% under target and 2% over target, the convergence varies uniformly between an extra 0.25% and a cut of 0.5%. ICBs between 2% and 4% over target have their base allocations reduced by 0.5%. Those over target by between 4% and 5.62% have reductions of between 0.5% and 0.94%, while those greater than 5.62% over target also have their base allocations cut by 0.94%.
In primary care allocations, systems with baselines more than 4.3% under target receive an additional 0.89%. The convergence factor for those between 4.3% under target and 1.59% over varies uniformly between an additional 0.89% and a cut of 0.4%. ICBs with baselines more than 1.59% above their primary care target allocations will be reduced by 0.4%.
Convergence has been adjusted to account for whether a system is a net importer or exporter of activity. Net exporters, where the provider cost base is smaller than the allocation, have fewer opportunities to achieve savings, while net importers have more opportunities, the national bodies explained. Sustainability funding previously paid to providers and commissioners will now be included in system budget allocations and subject to convergence over time.
In a change from previous years, in 2022/23 the baseline has been set using allocations for the second half of 2021/22 (H2), doubled to create a full year budget. It includes more than just clinical commissioning group allocations – CCG programme allocations, system top-ups (including sustainability funding and the Financial Recovery Fund), and growth funding are also now in its scope.
There are some adjustments – Covid-19 funding, CCG running cost and delegated primary care allocations are excluded and distributed separately. Other funding lines, including non-recurrent funding that was in the H2 funding envelope, such as for backpay for H1 following the 3% pay award, have also been excluded.
The guidance also notes that the 2021/22 baselines used to calculate the 2022/23 allocations include a mix of some provider-based and some population-based costs due to the structure of the Covid financial framework. It adds that a baseline exercise to move towards a population-base is planned before the 2023/24 allocations are issued.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.