‘Radical’ finance reform plans emerge

In a planning letter, NHS Improvement chief executive Ian Dalton (left) and his NHS England counterpart, Simon Stevens (below), said providers and commissioners will be required to submit one-year operational plans for 2019/20.
These will then be aggregated by sustainability and transformation partnerships and submitted alongside their new five-year strategic plans
next summer. Integrated care systems (ICSs) will also be required to submit agreed five-year strategic plans.
The letter said the new strategic plans will allow the bodies to consider the outputs of the long-term plan and the 2019 spending review capital settlement. Five-year commissioner allocations will be published in December.
Proposals for a one-year national tariff were also published, which committed to a move to a blended approach to payment in urgent and emergency care from 2019/20.
With break-even being the norm for all NHS organisations in the medium term, over time individual control totals would not be needed, allowing provider and commissioner sustainability funds to be phased out. The funds would be added to the baseline and initially targeted at urgent and emergency care (UEC).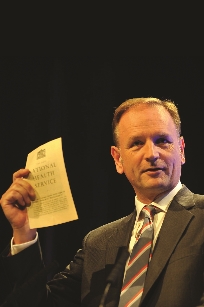
Both the marginal rate emergency tariff and the emergency readmissions rule will be removed – the national bodies said this would be on a cost neutral basis. The market forces factor will be revised, with a four-year transition to ensure it does not destabilise local health economies.
Speaking at the NHS Providers annual conference in October, Mr Dalton said these ‘radical’ changes could not be achieved overnight, but the transition would begin in 2019/20. Control totals will be retained next year, but rebased to make the figures more realistic at trust level.
‘From 1 April, I’d like to see the provider sustainability fund, which is £2.45bn, to be very significantly reduced, potentially by a 10-digit figure, with the funds released going directly into the UEC tariff price, which we know has been significantly underfunded. We also want to get rid of the illogical marginal rate, which means admissions are being paid at less than their cost, as well as 30-day readmissions fines. This sits in a context of wanting to move away from payment by results, towards blended payment mechanisms for urgent care which will enable trusts to more appropriately resource this high-growth area of service.’
The HFMA backed the one-year tariff for 2019/20, but believed tariffs should be set for two years or longer thereafter. It added that HFMA members tended to support blended payments for UEC as removing MRET and the readmission rule streamlined the payment system. The blended approach reimbursed the true variable nature of costs and acknowledged there was a cost when patients were readmitted.Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.