News / News review – June 2021
There was outrage in many quarters, and disappointment from NHS Providers, as the Department of Health and Social Care recommended NHS pay increases of 1% in 2021/22. In evidence to the NHS Pay Review Body and the review body for doctors and dentists, the Department said health budgets for the year had been set on an assumed pay rise of 1%. It pointed out that the government would increase the NHS pay bill by a further 0.7% due to the abolition of some transitional pay points for Agenda for Change staff in bands 5, 6 and 7. A commitment to maintain the pay of some staff in bands 8 and 9 would add further costs.
 The devolved administrations insisted they would not be tied to the 1% limit. In Northern Ireland, finance minister Conor Murphy said ministers would consider the recommendations of the pay review bodies before setting healthcare pay rises for 2021/22. The Welsh government also insisted there would be no 1% cap on uplifts. The Scottish government offered most local Agenda for Change staff a 4% pay uplift for 2021/22. The British Medical Association warned that the latest inflation figures (1.5% in April) showed a 1% award would amount to a pay cut in real terms.
The devolved administrations insisted they would not be tied to the 1% limit. In Northern Ireland, finance minister Conor Murphy said ministers would consider the recommendations of the pay review bodies before setting healthcare pay rises for 2021/22. The Welsh government also insisted there would be no 1% cap on uplifts. The Scottish government offered most local Agenda for Change staff a 4% pay uplift for 2021/22. The British Medical Association warned that the latest inflation figures (1.5% in April) showed a 1% award would amount to a pay cut in real terms.
There have been personnel changes in government following May’s elections. Humza Yousaf (pictured) succeeds Jeane Freeman as Scotland’s cabinet secretary for health and social care. He will have responsibility for the NHS, including the recovery of services as Scotland moves out of the pandemic, and the establishment of the new national care service. During the election, the SNP pledged to increase NHS frontline spending by at least 20% or more than £2.5bn to support recovery from Covid-19.
Meanwhile, in Wales, Eluned Morgan has been appointed minister for health and social services and will focus on NHS recovery and the pandemic response. Vaughan Gething, who had been in the job for five years, has become minister for the economy.
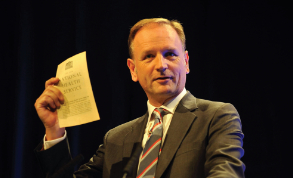
There will be a seismic change at the top of NHS England, as chief executive Simon Stevens (pictured) stands down at the end of July after more than seven years in the role. Not only has he led the NHS in England over the pandemic, but he has also steered the service through its biggest funding squeeze since the second world war and moved it towards a more integrated, collaborative model.
Lessons must be learnt from Covid-19 to better prepare the UK for future emergencies, the National Audit Office said in a report on the initial phase of the pandemic. The government has promised an inquiry into the Covid response next year, but in the meantime the NAO found that the UK was not as well prepared as it might have been. The report added that the pandemic had exacerbated existing fault lines in society, including inequalities, the need for social care reform, legacy IT issues, and the financial pressures on local government and the NHS.
The government published its white paper on integrating care – which included making integrated care systems (ICSs) statutory organisations – earlier in the year and its plans were confirmed in May’s Queen’s speech. It pledged to bring forward a health and care bill that will focus on integration and prevention. The speech, which outlines planned legislation over the coming year, added that additional funding will be provided for the NHS. The backlog of 4.7 million people on waiting lists would be addressed, and ‘missing referrals’ would be encouraged to see their GP.
NHS performance statistics show five million patients waiting to start treatment at the end of March. NHS Providers warned that full recovery could take three to five years. Chief executive Chris Hopson said that, together with additional government funding, a five-part strategy was needed to clear the Covid-related backlog in a reasonable time period. The five elements of the strategy included: increasing physical and workforce capacity; dealing with bottlenecks, such as investment in diagnostic hubs; making productivity and efficiency gains; reconfiguring hospitals so the NHS can deal with future Covid waves and winter pressures; and rapidly adopting new technologies to treat patients.
Welsh health and social services minister Eluned Morgan outlined plans to kick-start the local NHS pandemic recovery with an initial £100m. The funding will be used for equipment, staff, technology and new ways of working across all health sectors. The minister said it would increase capacity and cut waiting times as non-urgent care resumes. The Welsh government had committed £1bn overall to support its recovery plan.
Health pressure groups and others criticised the lack of plans for social care reform in the Queen’s speech. The Commons Health and Social Care Committee warned that ICSs could be destabilised if costed changes to social care are not brought forward soon. Chair Jeremy Hunt said the lack of social care changes was a ‘glaring omission’ in the government white paper on reform of health and social care. A committee report on the white paper added that greater clarity was needed on the governance of ICSs, including where the lines of responsibility would be drawn between the ICS NHS body and the ICS health and care partnership.
Planning guidance for the NHS in England in 2021/22 prioritises a number of areas, including Covid care, staff wellbeing, cancer and elective services recovery. The current payment arrangements based on block contracts will be retained over the first six months of the financial year (H1). There will be £1bn for elective recovery and £500m for mental health services recovery. NHS England confirmed a £160m initiative to accelerate the recovery of elective waiting lists by piloting new care models in 12 areas and five specialist children’s hospitals. The elective accelerators, as they will be known, will receive a share of the funding and additional support to implement and evaluate new approaches to increasing the volume of elective surgery. These will include a high-volume cataract service, one-stop testing, greater access to specialist advice for GPs and pop-up clinics.
The month in quotes
‘I am under no illusions about the size of the task ahead, but it is also important to recognise we now have a real opportunity to transform the delivery of health and care services. The pandemic saw the early and swift adoption of new technology and ways of working. I want to see health boards build on this good work.’
New Wales health minister Eluned Morgan (pictured) calls for change to speed up the recovery of health services
‘One of the challenges we’ve faced are the financial consequences of the pandemic. We’ve proposed what we think is affordable to make sure NHS people do get a pay rise.’
Health and social care secretary Matt Hancock defends the government’s proposed 1% pay rise
‘It’s hard to think of anyone who has had a more profound and positive impact on the NHS in its seven decades. He has also been a huge supporter of innovation, and has given the green light to NHS investment in a wide range of practical clinical improvements.’
Ara Darzi says Simon Stevens’ influence is unparalleled
‘Sir Simon has led the NHS with great distinction for the past seven years. I want to thank him for his dedicated service throughout – but especially when facing the extraordinary pressures of the past year, and for his huge contribution to our vaccine rollout.’
Boris Johnson leads the tributes to Simon Stevens
From the hfma
A range of blogs in Healthcare Finance weekly looked at environmental issues, integrated care system (ICS) governance, social impact bonds, year-end issues, the future of external audit and the role of non-executive directors (NEDs).
Sheffield Children’s NHS Foundation Trust finance director John Williams said finance must be at the heart of efforts to implement a net carbon zero NHS by 2040. Post-pandemic, there is an opportunity to consider the shape of the workplace, which could bring environmental and work-life balance benefits, he said.
Chesterfield Royal Hospital NHS Foundation Trust director of finance Lee Outhwaite said creating ICSs was about more than moving functions from one body to another. There will also be big changes in roles and how services are designed and run, he argued.
Emma Knowles, HFMA director of policy and communications, said more clarity was needed on ICS governance and lines of accountability, while Steve Connor, Mersey Internal Audit Agency managing director, said NEDs have a big part to play in the governance of ICSs.
Katy Nex, Social Finance end-of-life care integrator development manager, said social impact bonds could be a way of funding contracts to deliver improved outcomes.
With NHS finance professionals focused on the year-end, the HFMA’s Lisa Robertson anticipated a different audit process. While NHS bodies had to take account of new factors, such as temporary financial regimes, she said, the fundamentals still remained the same.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.