News review - May 2018
April brought some respite from the cold weather that hit the UK in March, when the Beast from the East at the beginning of the month and a shorter, though still icy, blast in the middle of the month kept up pressure on hospitals. So, it was not surprising when A&E performance figures for March were among the worst on record.
According to NHS England, in March A&E departments recorded the lowest performance figure against the four-hour waiting time target since the collection began. Figures showed 84.6% of patients were admitted, transferred or discharged within the four-hour target period. In February, this was 85% and in March 2017 the proportion was 90%. However, the cold weather meant A&Es saw more patients – attendances were 1.6% higher compared with March 2017. And attendances in the past 12 months were 2.2% up on the preceding year. However, delayed discharges continued to fall – in February, they were 25% lower than in February 2017.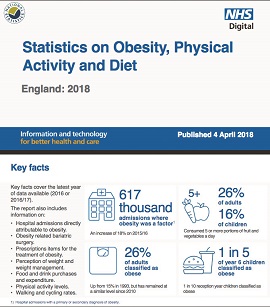
Of course, weather is not the only cause of demand and the NHS is seeing an increasing number of people whose ill health is due to their lifestyles. NHS Digital said hospital admissions where obesity is a factor increased by 18% in 2016/17 compared with the previous year. In total, there were 617,000 admissions to NHS hospitals where obesity was recorded as either a primary or secondary diagnosis. Of these, 10,705 had obesity recorded as the main cause – 9,929 up on 2015/16. The figures were included in the annual publication Statistics on obesity, physical activity and diet; England 2018. Adult obesity prevalence stood at 26% in 2016, a proportion that has been relatively constant since 2010. Child obesity prevalence was 10% in primary school reception year and 20% in year six.
The Department of Health and Social Care and its arm’s length bodies were unprepared for the Wannacry cyber attack last May, according to the Commons Public Accounts Committee. The committee’s report on the attack said the national NHS bodies had not shared or tested a response plan before the incident and no trust had passed a cyber security inspection. It added that there was much to be done to prepare for another attack and it was a case of when, not if, this would happen.
NHS England has provided a breakdown of the £114bn commissioning budget for 2018/19. NHS England funding and resource 2018/19 confirms clinical commissioning groups will receive £75.6bn, together with the new £400m commissioner sustainability fund (CSF). The CSF will support all CCGs to return to in-year financial balance. In addition, a further £32.5bn is being spent on direct commissioning, including general practice, while £2.5bn is held for the provider sustainability funds. The remainder will fund a range of transformation programmes, administration costs and other central programmes. NHS England’s running costs budget has been set at £508m – a real terms reduction after pay and price inflation.
The NHS in Wales must now comply with nurse staffing levels legislation. The Nurse staffing levels (Wales) Act requires health boards and NHS trusts to take steps to calculate and maintain appropriate nurse staffing levels in adult acute medical and surgical inpatient wards. The act also gives them a broader duty to consider how many nurses are necessary to provide care for patients sensitively in all settings.
The Welsh government also approved two new capital schemes at Hywel Dda University Health Board in March. It has given the green light to a £25m development of obstetric and neonatal facilities at Glangwili Hospital in Carmarthen. The development is due for completion by 2020. A £3m scheme to modernise haematology, oncology and palliative care at Withybush Hospital in Haverfordwest was also approved.
NHS Improvement announced that seven trusts will take part in a three-year Lean programme. The oversight body said the scheme would introduce a Lean management system in each of the trusts, building on the earlier partnership between the NHS and the US-based Virginia Mason Institute. The trusts will also build a network to share best practice across the NHS.
Scotland health secretary Shona Robison said the appointment of an interim chair and acting chief executive at NHS Tayside will increase financial scrutiny. The health board was placed in special measures in March over its leadership and the management of its finances. NHS Greater Glasgow and Clyde chair John Brown will also take up the role of interim chair at Tayside, while NHS Grampian chief executive Malcolm Wright will be acting chief executive. Mr Wright will retain his role at NHS Grampian.
More people would be given the right to a personal health budget or integrated personal budget under plans published by NHS England and the Department of Health and Social Care. Currently, people receiving continuing care have a right to a personal health budget, but the bodies said they would like to extend this right to a number of other groups. Where clinically appropriate, the newly eligible group would also have the right to an integrated health and social care budget. People with ongoing social care needs who also regularly access NHS services and people leaving the armed forces who are eligible for ongoing NHS services could be eligible for an integrated budget. A consultation on the proposals closes on 8 June.
NHS Providers warned regulators are not keeping pace with integration of care. Its survey of provider trusts showed just one in five were clear about how providers will be regulated. Respondents said they were unclear how regulators would approach oversight of sustainability and transformation partnerships and integrated care systems. NHS Providers said lack of clarity could lead to duplication of regulatory activity and confusion over which body holds trusts to account for financial performance and care quality locally.
A report on financial difficulties including a severe cash shortfall at Barking, Havering and Redbridge University Hospitals NHS Trust has highlighted issues in the financial governance of the trust. The trust has been reliant on external financial support for several years and had managed cash flow challenges by stretching creditor payments, leading to pressure from suppliers. The trust commissioned Grant Thornton to assess the causes of the cash problem and governance arrangements. Among the contributing factors were non-payment of activity over-performance by commissioners, divisional overspends and over-optimistic assumptions. It said there was insufficient escalation of the issues to the board and inadequate reporting. It recommended improvements to the trust-wide finance report including more detailed analysis of the balance sheet and cash flow with clear, concise explanations of the financial issues and risks. The trust said the report made ‘uncomfortable reading’ and the approach to financial reporting was being overhauled. ‘We have already made significant changes to the way we operate,’ it said.
Month in quotes
‘Government must get a grip on the vulnerabilities of and challenges facing local organisations, as well as the financial implications of Wannacry and future attacks across the NHS. Cyber security investment cannot be properly targeted unless this information is collected and understood.’
Commons Public Accounts Committee chair Meg Hillier (pictured) with a call to action on cyber security
‘The NHS simply cannot go on like this. Running a health system so close to capacity is highly risky and doing so endangers patient safety, as well as staff wellbeing.’
Nuffield Trust chief executive Nigel Edwards (pictured) says that despite a huge effort from the NHS, the winter has shown changes are needed
‘At a time when trusts are under tremendous pressure to meet ambitious financial targets, address workforce challenges and meet rising demand, it is disappointing to see the burden and the number of ad-hoc requests from regulators increase again.’
Amber Jabbal, head of policy at NHS Providers, says regulators must consider the impact of their requests for information
‘We now have a system to empower and support nurses on the frontline, and nurse leaders to use their professional judgement to understand and plan for the right levels of care.’
Wales health secretary Vaughan Gething describes nurse staffing legislation as a step forward
From the HFMA
Costing has moved forward a great deal in the last few years, but there is still work to be done if the NHS is to realise costing’s full potential. So says Catherine Mitchell, head of the HFMA Healthcare Costing for Value Institute. In a blog on the association website, she says that costing can be associated in many minds with crudely imposed budget cuts. But good cost data can prevent crude, top-down cuts – allowing cost improvement programmes to target waste and highlight areas for improvement.
Another new blog looks at accountants’ ethical responsibilities. Introducing a briefing on these duties for finance staff and other stakeholders, HFMA research manager Lisa Robertson says ethical responsibility is at the heart of an accountant’s role. Pressures can mount, particularly in a tough economic climate and as integration brings in new complexities and conflicts. The briefing examines NHS finance staff responsibilities and explores potential ethical dilemmas.
Trusts are increasingly interested in setting up wholly owned subsidiaries to deliver services such as estates and pharmacy. There is some controversy around subsidiaries, but, that aside, there are also many practical and accounting issues to consider when setting them up. HFMA policy and technical manager Debbie Paterson sets many of these out in a blog. The association has published a draft briefing considering some of the issues, including governance and general ledger and IT requirements, and has called for comments.
• To view any of the HFMA’s blogs, click here.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.