Extra funding for systems to implement long-term plan
Publishing its implementation framework for the long-term plan, the national body said the five-year clinical commissioning group allocations published in January were the starting point for system planning. (Read an HFMA summary of the implementation framework here.)
However, the allocations would be complemented with additional funding distributed to all systems on an indicative, fair shares basis. Alongside this, it will allocate targeted funding to be used to meet specific long-term plan commitments through regional and national programmes.
The funding will come in two parts – that available to all systems, and funds for specific programmes. In 2019/20, the additional funding allocated to all systems will total £538m and in the following years this will rise to £560m, £814m, £1.2bn and almost £1.78bn. The funding should be used to meet commitments on mental health, primary care and disease areas such as cancer, as well as helping the elderly age well.
The targeted funding is £418m in 2019/20, followed by £939m, £1.1bn, 1.25bn and £1.48bn. This funding will be used to meet long-term plan commitments on a range of areas, including:
- Digital first primary care support funding
- Revenue funding for provider digitisation and local health and care records
- Developing community services for adults and children with learning disabilities and autism.
All the additional funding will be conditional on agreeing five-year strategic plans rather than individual bidding rounds. The funds form part of the £20.5bn long-term settlement unveiled last year. To date, only CCG allocations have been announced.
Matt Tagney, long-term plan programme director, said: ‘We want to make as much of the funding tied to the single process of agreeing their plans to make it simpler and easier for them,’ he added.
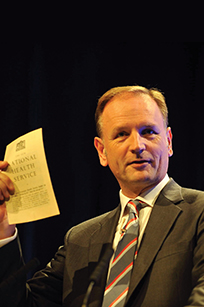 Asked if there was flexibility within the additional funding for systems to move money between priorities, NHS chief executive Simon Stevens (pictured) said: ‘Across the board, generally, yes but not on mental health and primary and community services because those typically have been the two parts that have been squeezed rather than over-invested in.
Asked if there was flexibility within the additional funding for systems to move money between priorities, NHS chief executive Simon Stevens (pictured) said: ‘Across the board, generally, yes but not on mental health and primary and community services because those typically have been the two parts that have been squeezed rather than over-invested in.
‘Frankly there is no part of the country that is currently doing so brilliantly on its mental health service that we can say, “Take the foot off the gas and at the margin use what was for mental health for something else”.’
Draft plans will be shared with regions in mid-September, with final plans agreed with system leads and regional teams by the end of October. NHS England and Improvement will publish a national implementation plan in December.
The framework also set out indicative financial planning assumptions to consider when developing strategic plans. The assumptions cover pay, non-pay and drugs costs, together with the indicative tariff uplift. Strategic plans should explicitly set out how the additional funding being invested will deliver real improvements for their populations.
NHS Providers welcomed ‘much needed clarity’ for local NHS leaders. Chief executive Chris Hopson said: ‘We must, though, be realistic about how much can be delivered for the extra money provided alongside the long-term plan – given how far the NHS has fallen behind existing performance standards, the scale of workforce gaps, the need to deliver more integrated care and the sheer breadth of what we are seeking to deliver for patients.’
NHS England and NHS Improvement will work with the NHS over the coming months and set out further details of the financial framework for 2020/21 and later years.
Other areas identified for further work include the NHS capital regime, workforce development and primary care network and community services development.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.