Making it real
Population health management – using data to guide the planning of care and support to achieve the maximum impact on the different groups of people that make up local populations – is a major buzz phrase at the moment. It featured heavily in the NHS long-term plan and local systems dutifully took up the challenge, putting it at the heart of refreshed strategic delivery plans.
But while it is one thing to recognise the value of using data to help shape the right response to improve the health of different cohorts of patients and the population, putting it into practice is a difficult proposition. It requires the pulling together of multiple data sets and finding ways to share that data with the teams that can decipher what the data is saying and revise pathways accordingly.
A new tool developed by Leeds Teaching Hospitals NHS Trust may just provide a practical step forward and help clinical teams to start asking the right questions.
The trust’s director of finance, Simon Worthington, says the idea is to look at cohorts of people who are or will become patients and look for ways to change outcomes proactively, taking account of all the wider determinants of health. ‘This is not a new approach,’ he says. ‘But being able to do it practically has been really difficult.’
Finding a practical way to address this is important for Leeds, as a move to population health management is at the heart of the city’s plan for improved health and wellbeing. A ‘left shift’ of resources upstream could mean that expanded hospital services are not necessary.
Developed by the costing team, the PLICS population health management analyser marries patient-level cost data with comorbidity and lifestyle information drawn from the trust’s own patient data and from the Office for National Statistics.
The result is a tool (pictured) that can be used by clinicians and others to explore the resources being consumed by different parts of the population.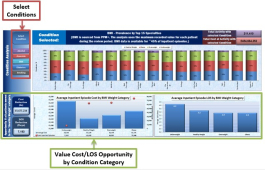
It starts at a very high level showing the cost and population distribution across the city. Users can look at a high level across the whole city. For example, this reveals that, while each of the city’s 33 wards has between 2.4% and 4.8% of the total population, resources spent on those communities range from 1% to 4.3% of overall costs. They can also analyse this by age, finding that while over-84-year-olds account for just 2% of the population, they consume nearly 6.8% of total resources.
Pulling in ONS data on the index of multiple deprivation (IMD) also highlights the disproportionate spend on people living in the most deprived parts of the city.
Users can then drill into the data, analysing the resources consumed at either ward or primary care network (PCN) level.
The analyser (pictured) also highlights overarching figures on the public health context. For example, it can show levels of smoking or diabetes per 100,000 for each specific ward, putting this alongside other relevant information such as the outpatient did-not-attend rate for that ward and the associated households in that ward without a car.
Access to more data
However, this is only half the story. Arguably the real power of the tool comes from pulling in the trust’s own data on lifestyle issues such as smoking status, body mass index (BMI), anaemia, diabetes and alcohol consumption.
This data is not currently available for all the trust’s patients, but the costing team discovered it had access to far more data than it had initially realised. It hopes that showing the value of having this data could lead to more comprehensive collection.
This separate analysis allows users to look at activity by specialty or geographic location through the lens of these different conditions and lifestyle issues. So, it will show you the split of activity in each specialty by BMI – healthy weight, obese, overweight or underweight.
It also shows the average inpatient costs for different specialties, such as cardiology or gastroenterology, and average length of stay by these different BMI categories.
An opportunity calculator will then show an indicative potential reduction in costs or length of stay that could be achieved if all patients moved to the ‘healthy weight’ category.
Vinod Bassi, assistant director of finance for business support and costing, says the tool doesn’t answer the questions on how to improve health for different cohorts of patients. ‘But it informs the questions that should be asked,’ he says.
‘By identifying the potential opportunities, you can start to ask how you might influence lifestyles. If you want to explore the impact that reducing smoking among gastroenterology patients could have, you can quickly see it.’
It is not about saving money – the cost data is just another patient-level dataset that contributes to the overall picture. But it can add to the case for making public health interventions to address lifestyle issues before patients come into hospital.
For example, anaemic patients tend to exhibit higher costs and longer lengths of stay. And it turns out that the trust will typically have the data on a patient’s iron levels from blood tests, but previously has not made use of this information.
Iron deficiency can often be improved prior to a planned inpatient episode, but this requires changes to pathways.
Mr Bassi says that, although the tool is in its infancy, the response from clinicians has been positive. ‘It is generating real enthusiasm and excitement,’ he says.
One such clinician is Sophie Blow (pictured), an advanced clinical pharmacist at the trust with a focus on perioperative optimisation. She says that many of the things that could improve outcomes are related to comorbidities.
‘But we struggle with knowing the numbers of patients we have with various conditions, where they come from and how to target them,’ she says. ‘[We want to know if we] can do patient-centred care rather than just take a blanket approach.’
Being able to drill down into PCN level – the trust covers 19 PCNs – provides real insight. ‘We have three PCNs that provide approximately 25% of our elective surgical patients and we can see that they account for among the largest numbers of smokers,’ says Ms Blow.
The trust has access to a smoking cessation resource from Leeds City Council, although it is not currently used in a focused way. However, information provided by the analyser shows the potential benefits of targeting this resource at areas where it will have most impact.
Equally, it could be targeted at specific surgical interventions – there is a major link between urology and bowel cancer outcomes and smoking status, for example.
Ms Blow says changing smoking status, even a few weeks before an operation, can have a major impact on length of stay. ‘It is different for different specialties, but most smokers will stay an extra day in hospital.’ Reducing this is better for the patient and, in terms of freeing up capacity and reducing costs, it is a significant efficiency.
‘It also gives the patient something they can do to support their surgical outcome and starts to build a partnership between the medical team and the patient,’ she adds. ‘[The tool] has opened doors for us and given us opportunities that we just never had before.’
Added value
Martyn Robertson (pictured) is an anaesthetics consultant with an interest in perioperative medicine at the trust. He agrees that the tool could become a really valuable resource, pulling reliable data sources together into a single place and making it analysable.
‘It is really useful putting pound signs next to things,’ he says, ‘it gives you a potential. For example, if all the trust’s cystectomy patients became ex-smokers from current smokers, how much would that save you from a surgical inpatient stay?’
Dr Robertson continues. ‘And that is just the seven days in hospital.’ If you add in the potential downstream benefits of making that earlier intervention, the patient and financial benefits really start to accrue.
Fellow consultant anaesthetist Alwyn Kotze agrees. ‘[When you look at it like this] the preoperative assessment, which we’ve always thought of as a way of preparing for surgery, becomes just another opportunity for improving long-term health,’ he says. While patient-level data has always allowed clinicians to drill into hospital data, the new tool ‘allows us to look at the community impact’, he adds.
Management and the board is also excited, seeing it as a practical way to further the trust’s and wider system’s population health management goals. And with many of the actions to improve population health likely to involve system responses, clinical commissioning groups have also been briefed about the new analyser.
Rob Newton, the trust’s associate director of policy and partnerships, says non-elective admissions are rising in most health systems, driven by comorbidities. It is also well known that comorbidities are more prevalent in deprived areas. Typically, the inequality situation is expressed in terms of differences in years of life expectancy – often from a commissioner’s perspective.
‘The appeal of presenting information [in this way] is that we can see what inequality looks like from the trust perspective,’ he says. ‘If we go into our emergency department, we can use our own data to look at the direct impact of inequality. There is a real strength in being able to articulate this for us.’
Mr Worthington is convinced that the way the tool has been created, meeting specific requests from clinicians, will be key to its future success.
‘As we move forward, this will be a really helpful tool and most of the work will be bottom up – that’s the power of it,’ he says.
Doctors of data
Vinod Bassi (pictured right), assistant director of finance at Leeds, says that costing practitioners have to be ‘doctors of data’ and make people aware of their data processing skills as well as their traditional finance competencies.
The trust’s costing team includes a dedicated information manager who has passed on SQL programming skills to his colleagues. ‘This has enabled us to access, extract and combine data in trust servers ourselves, rather than relying on the informatics department,’ he says.
‘Our philosophy is that we are privileged to have access to mountains of data that we use as part of our monthly patient-level cost production cycle. Using this to its fullest potential has meant that we have had to develop and evolve our analytical capability to convey what the information is saying to the people we are working with, so that they can drill into it and investigate the issues they are trying to examine.’
Awareness of the broader capabilities of the costing team have grown over the last couple of years, partly thanks to the team’s Twitter account @LTHTCostingTeam.
The PHM tool grew primarily out of two initiatives. The team undertook some work to support a local anaemia collaborative. The collaborative wanted to improve the preoperative treatment of people with anaemia, which evidence showed would lead to lower length of stay and lower rates of blood transfusion. But it needed to be able to evidence the improvements that could be made to encourage roll-out among different surgical specialities.
Tom Mitchell (pictured left), cost accountant at the trust, said the challenge was linking to the right data. Coding for anaemia was poor, so a different source was needed. The costing team was used to matching blood tests to patients, to apportion costs. Now it realised it could also access the test results, providing a clear view of patients’ anaemia status. And this enabled the trust to establish a baseline position against which improvements could be tracked.
On the back of this, other clinicians started approaching the team with requests for data to support their own improvement programmes. Another major step forward came with a project to explore the benefits of capturing more lifestyle information on the trust’s electronic medical record PPM+. The team was given access to some data from the Perioperative Quality Improvement Programme (PQIP) research database, which contained diabetes and smoking status, height and weight and anaemia results for a large sample of patients involved in research programmes.
It created a PQIP analyser and dashboard that linked all this lifestyle and condition data to costing data as a way of proving the concept. The commissioning clinician Martyn Robertson was thrilled, but things took off when trust finance director Simon Worthington saw the work. Recognising the potential to support the trust’s population health ambitions, he asked the team to explore what data they could pull together using their own and available national data.
Mr Mitchell said that the real lightbulb moment came with the realisation that the trust had its own data on patients’ lifestyle and conditions. ‘There is so much in the back end, although sometimes we needed help from clinicians to find it,’ he says. ‘But once you’ve located it, if you have the SQL skills, the results can be revolutionary when you connect it back up to patient cost data.’
It is not comprehensive, but it is extensive enough to inform decisions. For example, the trust has smoking and height/weight data for around 45% of its patients. Alcohol consumption data is lower at 20% but anaemia is high at 79%. Patients’ diabetes status is comprehensive because it is included in clinical diagnosis codes. And the trust feels that this position can be improved as more people understand the wider benefits of collecting the data.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.