Feature / Costing tour
In April, NHS Improvement published its first healthcare costing standards to set out a consistent methodology for compiling patient-level costs in acute provider bodies. These standards are not mandatory and are still in draft format. However, the clear aim is that in future all providers – initially in the acute sector but then moving on to cover ambulance, mental health and community providers – will be required to adhere to the standards.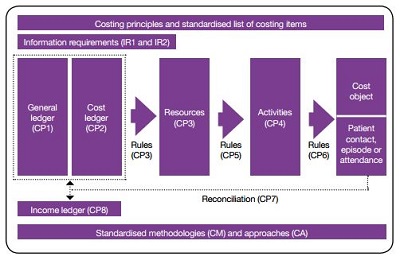
NHS Improvement’s costing transformation programme (CTP) is following a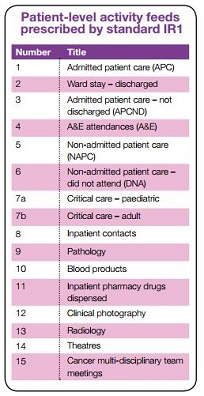 staggered timetable. The first mandatory collection for all acute providers will be in July 2019, with all providers joining in by July 2021.
staggered timetable. The first mandatory collection for all acute providers will be in July 2019, with all providers joining in by July 2021.
This may seem a long time away, but the timetable is ambitious, with providers across different sectors and within each sector facing a different scale of challenge. This will depend on their starting position in terms of existing systems, source data and staff engagement (including clinical staff).
No-one can afford to postpone getting to grips with the new costing approach as set out in the new standards. Getting some familiarity with the key components – and how the approach differs from existing costing methodology – is a fundamental starting point. Alongside eight costing principles, there are 24 standards in the following categories:
- Information requirements (2)
- Processes (8)
- Methodologies (9)
- Approaches (5).
Below are a few highlights from these standards, along with explanations of some of the ‘new’ concepts and language being used.
Information requirements
Costing begins with good-quality source activity data. The information requirements standards describe the activity information required to implement the other costing standards. And they set out how costing teams can work with informatics and service departments to obtain good-quality data for costing. These standards should be shared with the informatics department and departments providing activity data for costing.
Standard IR1: collecting information for costing purposes
The CTP aims to standardise the collection and use of information in costing. This standard prescribes the minimum 15 patient-level feeds (see table left) for implementing the standards. As providers may not currently collect all this information, a lead-in time may be required before all of it is available for costing. NHS Improvement also recognises that these 15 patient-level feeds do not cover all the activity a provider delivers.
Costing processes
The costing processes standards explain the steps of the costing process, from recording information in the general ledger through to producing the final patient unit cost and reconciling reported costs to audited accounts. The process standards should be applied to all the services provided by an organisation.
Standard CP2: producing a cost ledger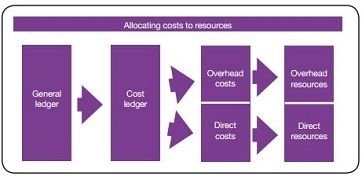
‘Cost ledger’ is new terminology for the costing process. As the general ledger is not generally set up for the costing process, most costing practitioners will need to move costs to their correct starting positions for costing. ‘Cost ledger’ just puts a name to this preparation work.
The purpose of the cost ledger is to ensure the costs are aggregated or disaggregated to the appropriate level to start the costing process and to ensure all costs are in the correct ‘starting position’ for the costing process. For example, where the general ledger separately identifies pay, pension, national insurance and overtime, these are combined into a single staff cost for the cost ledger.
On the other hand some costs need to be disaggregated. A subjective code in the general ledger containing nursing costs for different categories of nurse needs to separated into: specialist nurse; qualified nurse; and midwife.
A chart of accounts for the cost ledger will be published in the first version of acute costing standards to be published in January.
Standard CP3: allocating costs to identified resources
Costs from the cost ledger are first allocated to resources – the components used to deliver healthcare activities. Costs are mapped either to a direct resource (such as staffing, supplies or systems) or to an overhead resource (such as finance, human resources, estates or portering). The standard provides the prescribed list of resources. Costs do not need to be allocated against every resource listed, just against those that are most appropriate. Organisations will need to have the ability to report patient-level costs at both a resource group level (for example, ‘devices, implants and prostheses’) and at an individual resource level (for example, ‘heart valves’ or ‘hearing aids’).
Standard CP4: identifying activities
Resources must be mapped to a list of prescribed activities, but the first step is for costing practitioners to identify their own organisation’s activities and map these to the prescribed list. The 15 patient-level feeds prescribed in the information requirements standards do not cover all the activities performed by acute providers. However, all activities should be mapped to the prescribed list of activities and costed regardless of whether they are supported by a patient-level feed or not. An example of an activity group might be ‘chemotherapy’, containing separately identified activities of ‘drug issue’, ‘nursing clinical supervision’ and ‘pharmacy dispensation’.
Standard CP5: allocating resources to activities
This standard provides the costing allocation methodology for each resource and activity combination. There is only one prescribed allocation method for each combination. This is important to ensure that the costing process is standardised as far as possible to allow meaningful benchmarking.
NHS Improvement understands that providers may not be able to meet the prescribed costing allocation methodology immediately. In this case, providers may use a locally relevant methodology and document this in their costing manual.
Providers will also need to demonstrate they are working towards achieving the prescribed allocation methodology.
It is also the case that providers may be using superior allocation methodologies to those prescribed in the standards. A list of ‘superior’ costing methodologies is currently being compiled. Again, providers should document in their costing manual where they have used a ‘superior’ method. A list of costing methodologies that will not be accepted as superior or as local workarounds is also being produced and this will include using income or national averages to weight costs.
Standard CP6: matching activities to cost objects
Matching costed activities to inpatient episodes, outpatient attendances and contacts is crucial for accurate patient unit costs. An aim of the CTP is to standardise the costing process at every stage. This ensures that the results can be benchmarked as any cost variation will be due to service delivery decisions rather than variation in the costing methodologies used to calculate the costs.
Prescribed matching rules will reduce ‘false-positive’ matches – when the costed activity is not matched to the event it took place in. These rules will continue to be refined as the process is complex, with each activity potentially taking place in many different care scenarios.
The matching principles depart from current practice. Unmatched costed activities should not be absorbed by patients who did not incur these costs. The true cost of any procedure will never be established if patient unit costs are inflated by costs that were not incurred during the delivery of that procedure.
There will inevitably be some costed activities that do not match. Either the activity took place too long before the episode/contact/attendance, or the information in the activity feed is so poor that an appropriate match cannot be found.
Unmatched activity should not be assigned to other patient contacts, episodes or attendances.
To achieve consistent and comparable costing outputs, unmatched activity must be treated consistently across providers. This means the following rules must apply for any unmatched activity:
- If the specialty that ordered the item is identified but the item cannot be matched to a patient episode, contact or attendance, the cost sits in the specialty under reconciliation items. It should not be matched to the other patients in that specialty.
- If the specialty that ordered the item cannot be identified, the cost sits in the providing department under reconciliation items. For example, if a pathology test cannot be matched to a patient contact, episode or attendance and the requesting specialty (for example cardiology) cannot be identified, the unmatched activity would be reported under pathology as a reconciling item. This rule helps identify data quality issues.
The volume of unmatched costed activity is a good measure of the accuracy of the data used for costing purposes. It is an aim of the CTP to improve the quality of this data.
Reports of unmatched costed activity and the reasons why they could not be matched can be helpful in illustrating to informatics and other departments the importance of good-quality data to costing. As data quality improves, unmatched costed activities can be expected to reduce.
It is appropriate that some costed activities are not matched to any inpatient episodes, attendances or contacts because they were not part of this care. This could include activities relating to patients not in the provider’s care, including direct access activity and activity conducted on behalf of other providers. The cost group ‘reconciliation items’ has been adopted to record these costed activities so patient unit costs are not inflated.
Costing methodologies
The costing methodology standards provide guidance on how to cost high volume and high value areas within an organisation. These supplement the costing process standards.
Standard CM1: allocating overheads
This standard adopts approaches that depart from current practice. The first difference is that costs are classified as either patient facing or supporting, the indirect classification is not used.
Costs are driven in two ways only: by the cost objects (direct) or by other resources/activities (overhead/supporting). The indirect classification relates to organisation structure, not how costing is undertaken. Its inclusion is a management classification, which is separate and should be achievable by attributing the different resources/activities in the model.
For example, the cost of a radiology scan can be directly attributed to those patients who were scanned. Within costing, it is directly driven by the cost objects. For management purposes, it is an indirect cost as the scan is a clinical support service provided at the request of a main specialty such as trauma and orthopaedics.
We have adopted three different ways to allocate overheads to cost components. This is because detailed analysis of the overheads indicated that a one-size-fits-all approach does not accurately reflect how overhead costs are incurred. The use of three methodologies attempts to allocate overheads at the appropriate point in the costing process.
Standard CM7: theatres
Although it is not the approach used by many providers, this standard requires sessional costing as it addresses challenges in costing theatres such as overruns and cancellations. It is seen as a starting point for investigating the methodologies to include in future versions of the standards that more accurately cost overruns and underruns, as well as out-of-hours and emergency theatre work.
Standard CM8: critical care
Critical care nursing costs should be allocated using length of stay weighted by acuity, not the number of organs supported. The results using this methodology are being reviewed as the costing standards are implemented by roadmap partners. While the standards set out a hypothetical example of how weightings might look for different levels of acuity in critical care, the standards call for the development of local relative weight tables in each provider. A relative weight table should also be used to allocate non-pay costs. Medical costs should be allocated across all patients based on length of stay without an acuity weighting.
Julia Gray is costing standards lead at NHS Improvement
Patient-level activity feeds prescribed by standard IR1
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.