Costing: community progress
NHS England and NHS Improvement’s deadlines for its Costing Transformation Programme – now known as National Cost Collections – are demanding for all NHS providers. But it is providers of community services that arguably face the biggest challenges. Gloucestershire Care Services NHS Trust perhaps offers some encouragement about how much can be achieved in a relatively short period of time.
Acute providers will this year make their first mandated submission of patient-level costs covering admitted patient care, outpatients and A&E. Next year, they will be joined by mental health trusts and ambulance trusts. And it is likely that providers of community services – including acute and mental health providers also delivering community services and dedicated community service trusts – will be required to submit patient-level costs from 2021 (covering 2020/21).
costs covering admitted patient care, outpatients and A&E. Next year, they will be joined by mental health trusts and ambulance trusts. And it is likely that providers of community services – including acute and mental health providers also delivering community services and dedicated community service trusts – will be required to submit patient-level costs from 2021 (covering 2020/21).
The whole of the NHS has found this demanding. Trusts have had to move away from a top-down, allocative approach where they report average costs of a specified currency (healthcare resource groups or outpatient appointments in acute care or therapist/nurse contacts, for example, in community services). And they’ve replaced this with a bottom-up approach – building up and reporting the specific costs of treating individual patients. But the lack of electronically captured activity data, and a lower national profile for costing generally, has given community service providers a bigger mountain to climb.
Even understanding what constitutes a community service has proved quite challenging, although four out of five NHS providers deliver some form of community services and together they constitute about 10% of total NHS spend.The experience of Gloucestershire Care Services NHS Trust demonstrates that, even over a short time period, real transformative change is possible in community sector costing. ‘Before the changes were made, our costing data wasn’t used at all in any meaningful way,’ says Jenny Richards (pictured), costing accountant at the trust, which has more than 1.2 million contacts with service users each year and runs seven community hospitals.
 There was no real way to validate activity data and very limited engagement outside of the finance team. ‘The focus was on meeting the mandated reference costs, the reference cost index and satisfying ourselves that we understood any key movements,’ she says.
There was no real way to validate activity data and very limited engagement outside of the finance team. ‘The focus was on meeting the mandated reference costs, the reference cost index and satisfying ourselves that we understood any key movements,’ she says.
Fast forward a couple of years and the trust is one of the pioneers of patient-level costing in the community sector. As one of NHS Improvement’s roadmap partners since 2017, it has helped shape the development of community costing standards, made two reference cost submissions using a patient-level methodology and taken part in a national voluntary patient-level cost submission using the new centrally set methodology.
More than this, it has started to use the more granular data to challenge existing clinical practice and inform decision-making.
The trust’s patient-level cost journey began in earnest in January 2017, when it bought the Civica CostMaster costing system and signed up to become a roadmap partner. But it was starting from solid ground. ‘One of the key foundations is to have an electronic clinical system recording contacts and activity,’ says Steven Wainwright, the trust’s commercial manager. And the trust had just spent two years rolling out the SystmOne clinical system across the trust, with practitioners and community teams using mobile devices to input contact data. At the time, the then soon-to-be-published community services data set also helped firm up what the trust had to collect to meet central requirements.
Close collaboration between costing and analytic team colleagues led to the specification and implementation of a ‘bible’ to deliver automated activity datasets to support costing calculations and subsequent desired internal reporting.
Even so, the fact that the trust was able to make its reference cost submission in July the same year, based on patient-level data – with costs for 75% of services available at the patient level – was an impressive turnaround. Especially given its costing resource amounts to less than one whole-time member of staff.
‘There were two distinct phases,’ says Mrs Richards. ‘We made our original reference cost submission using our existing method but built up at patient level.’
Clinician pay costs were attributed to patients in proportion to the duration of clinician contact time with the patient, as recorded on the relevant electronic clinical system. This, importantly, created a direct link between the cost results and the patient clinical record.
‘We made the conscious decision to share results early with our clinicians, clearly setting expectations that the data would not be perfect, and that their input would be invaluable,’ says Mrs Richards. ‘This has proved successful as service leads have helped us and continue to help us to iteratively improve the quality of costing data.’
The 75% patient-level mark was reached by focusing on the major service areas where the trust was confident of its data – adult and non-specialist services. This approach continued in 2018, adding in specialist nursing and specialist services as well as children’s, dental health and sexual health services. This meant that the trust’s costs were now 98% at the patient level.
The trust identifies a separate, second phase where it started to apply the new Costing Transformation Programme (CTP) patient-level costing methodology developed by NHS Improvement, involving the breaking down of costs into resources and then activities. In January this year, the trust made a voluntary ‘proof of concept’ patient-level submission, reflecting the new methodology and using a new version of the CostMaster software.
While the trust still needs to file its 2018/19 reference cost
submission, it is also working towards a further voluntary CTP patient-level submission later in the year, when it hopes to submit costs for all in-scope activity alongside a wider group of early implementer community service providers (see Sector view, page 22).
Mr Wainwright stresses that it is an iterative process and that getting started and getting people engaged should be priorities for all trusts. Some jobs are time-consuming – mapping the finance ledger to the cost ledger, although this is largely a one-off piece of work and a crucial building block. And the sooner you share and analyse the results, the sooner you can iron out issues.
Identifying inconsistencies
‘There is nowhere to hide at the patient-level,’ he says. ‘Data quality issues are uncovered, giving you the opportunity to address them.
‘For example, patient-level scrutiny of the activity data for the trust’s integrated community teams identified inconsistent recording of some contacts across the distinct district nursing, occupational therapy and physiotherapy services. Subsequent close collaboration with operational colleagues has largely eliminated this, and improved the accuracy of recorded activity across the three services by different professional staff groups.’
While the focus has been on getting the data into a useable format and improving clinicians’ and operational teams’ confidence in the data, the organisation has also started to put the more granular data into use.
One area the trust has explored has been to examine the variation in how services are delivered across its five localities. ‘Operational leads are starting to look at a wider dataset to understand how they are deploying different bands of clinicians across different localities to administer the same type of care,’ says Mrs Richards. With district nursing contacts also broken down by type of contact (including diabetes, continence, respiratory and cancer), operational teams are starting to understand how pathways look in different areas.
Knock-on impact
Other service leads, motivated by the work with the district nursing service, are now looking for a similar breakdown. For example, currently occupational and physiotherapy contacts are only identified as first or follow-up appointments and whether the contact was face-to-face or not. SystmOne is now being revised to enable a more granular analysis. ‘That will mean we can have the same conversations about OT and physio to understand how the same interventions are delivered by different people in different localities,’ says Mrs Richards.
The analysis by locality has gained a level of sophistication. For example, with a wide-ranging skill mix across services in different localities, there are many different costs per contact. But looking at the same data by episode shows that the locality with one of the highest costs per contact has the lowest cost per episode. This gives operational teams a real opportunity to compare their service delivery approaches and optimise the approach across the whole health economy.
A powerful tool for clinicians has been charts showing different patient journeys and how disjointed they can be (see example). ‘When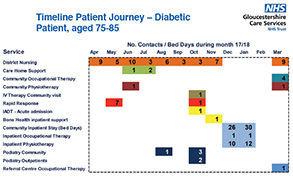 you show this to operational leaders and then put in the pound signs highlighting this has an annual cost of £30,000, it can stimulate debate around opportunities to improve patient outcomes and experience,’ says Mrs Richards.
you show this to operational leaders and then put in the pound signs highlighting this has an annual cost of £30,000, it can stimulate debate around opportunities to improve patient outcomes and experience,’ says Mrs Richards.
Even insights such as the £350 it costs to keep each of the 200 inpatient beds open each day can motivate teams to review pathways.
The ultimate goal is to develop this pathway view across the whole health economy. ‘We have a local population health approach that the Gloucestershire Integrated Care System is working on and the aim is to be able to report our use of resource by locality, looking at how a patient touches all our services – acute, mental health, community and ideally primary care – in a year. We want to build up a picture for the whole county,’ says Mr Wainwright.
That vision remains some way off and there are a number of information governance issues to overcome. But with a common patient identifier in the NHS number and all sectors now developing patient-level cost data, it is seen as a realistic target.
Sector view
Subject to consultation later in the year, community trusts may be required to make their first mandatory patient-level cost submission during 2021. With some trusts still needing to implement appropriate costing systems, IT hardware challenges (see Healthcare Finance, May 2019, page 14) and often small costing teams, NHS England and NHS Improvement recognises this is a challenging agenda.
However, the Costing Transformation Programme – or National Cost Collections, to give it its new title – is no stranger to big challenges. In getting to the point where all acute providers will submit patient-level costs this summer, the service has met a number of similarly demanding deadlines. And the experience of trusts such as Gloucestershire Care Services NHS Trust (see main feature) shows what can be achieved in a relatively short period of time.
Community service providers – both those providing services alongside acute or mental health services and those focused solely on community provision – have been aware of the timetable since the programme began. And there is a lot of guidance and support that they can draw on.
The healthcare costing standards – which set out a consistent approach to patient-level costing – have been published where possible as integrated standards relevant to providers in any sector.
In addition there is community sector specific guidance on the information requirements and some costing methods, including the costing of sexual health services, dental services and wheelchair services (with audiology being considered for possible further guidance next year).
Early implementers can also access NHS England and NHS Improvement’s online learning platform, which provides additional examples to supplement the standards. Trusts have the opportunity to participate in a voluntary collection during 2019.
However, for providers not yet in a position to participate, the advice is to start looking at all the resources available.
 Fiona Boyle (pictured), the programme’s community services costing manager, suggests there are different challenges facing integrated and dedicated providers of community services. ‘For many integrated acute and community providers, there is a focus on acute activity to ensure they can meet their first mandated submission in 2019,’ she says. ‘So, while they may have systems in place and reasonably sized costing teams, their attention can be on other areas and there may be a preoccupation with national tariff type issues. For the dedicated community provider, it may not have a suitable costing system or clinical system in place and costing resources can often be less than one whole time equivalent.’
Fiona Boyle (pictured), the programme’s community services costing manager, suggests there are different challenges facing integrated and dedicated providers of community services. ‘For many integrated acute and community providers, there is a focus on acute activity to ensure they can meet their first mandated submission in 2019,’ she says. ‘So, while they may have systems in place and reasonably sized costing teams, their attention can be on other areas and there may be a preoccupation with national tariff type issues. For the dedicated community provider, it may not have a suitable costing system or clinical system in place and costing resources can often be less than one whole time equivalent.’
All of this adds up to a case for getting costing on the agenda now. Given the lead times for tendering processes, Ms Boyle believes that system requirements need to be a priority. Beyond that, costing teams should ensure they are familiar with the guidance and make a start on mapping their finance ledgers to cost ledgers, so that they have the right starting position for the costing process.
Three community providers took part in January’s voluntary submission of patient-level costs and more than 25 have signed up for this year’s voluntary submission in the autumn, this time including integrated acute and community and mental health and community providers.
In 2021, a total of roughly 180 trusts (out of 227) are expected to be submitting costs for some form of community activity.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.