A fresh approach
The publication of refreshed planning guidance for 2018/19 was welcomed across the NHS. This was not only because local health economies have been waiting since November’s Budget for details about how additional funds will be shared out. It was also because the guidance brought with it some extra good news – a further increase in the resources available to local bodies and some pragmatic decisions about what the service can deliver, even with those increased funds.
But while there may have been a small sigh of relief, it stills leaves the NHS with a huge mountain to climb – as numerous commentators were quick to point out.
‘At least this is realistic,’ says NHS Confederation chief executive Niall Dickson. ‘To have expected the NHS to deliver more than has been achieved this year would have been to raise expectations and place further burdens on frontline care. It will be an immense task just to stabilise the service in the coming financial year.’
Saffron Cordey (pictured), director of policy and strategy and deputy chief executive of NHS Providers, adds: ‘Holding performance and meeting the required financial task is at the top end of what can be expected.’
The realism that both commentators refer to is a rolling forward of access targets by a year. In aggregate, providers will need to be seeing 90% of A&E attenders within four hours by September 2018, with a majority then achieving 95% by March 2019 and a complete return to the 95% performance standard during 2019. On elective surgery, health economies should target a reduction in the number of patients waiting over 52 weeks and the number of patients on an incomplete pathway should be no higher in March 2019 than in March 2018.
NHS England’s board paper said that allocations for 2018/19 allowed for a non-elective increase of 2.3% and 1.1% in A&E attendances – although growth patterns would vary by commissioner and provider.
However, hidden in the overall 2.3% figure was a trend of more modest growth for admissions needing an overnight stay in hospital and much higher levels of growth involving zero-day non-elective spells.
CCGs will also be given incentives to moderate demand for emergency care, with £210m of their quality premium funding contingent on managing growth in line with the agreed plan.
For electives, the assumption is that outpatient attendances will increase by 4.9% and elective admissions by 3.6%.
Perhaps the key trigger for refreshed planning guidance – given that the NHS already has two-year contracts in place based on two-year planning guidance issued in September 2016 – was the additional £1.6bn announced in November’s Budget for 2018/19.
In unveiling how this will be distributed, Refreshing NHS plans for 2018/19 – published jointly by NHS England and NHS Improvement – also adds an additional £540m into the mix, made available by the Department of Health and Social Care.
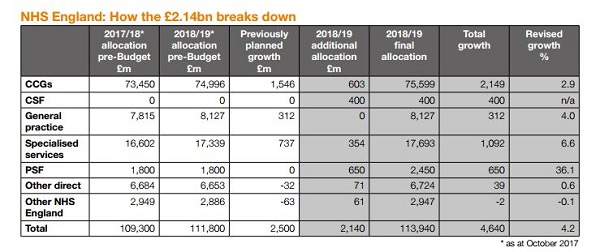
That means an increase of £2.14bn compared with the 2015 spending review figure for 2018/19. Total growth compared with 2017/18 (not taking account of the non-recurrent additional funding for 2017/18 announced in the Budget) now amounts to £4.6bn, equivalent to 4.2% cash or 2.4% in real terms.
The extra £2.14bn breaks down into an additional £603m for clinical commissioning groups, with a further £400m creating a commissioner sustainability fund (CSF). Specialised services receive an additional £354m and the provider sustainability fund (PSF, a rebrand of the former sustainability and transformation fund) gets a further £650m on top of its existing £1.8bn (see table).
In fact, NHS England says the resources available to CCGs will increase by £1.4bn – enabling them to fund ‘realistic levels of emergency activity in plans, the additional elective activity necessary to tackle waiting lists, universal adherence to the mental health investment standard and transformation commitments for cancer services and primary care’.
On top of the £603m increase in allocations and the new £400m CSF, NHS England has removed the requirement for CCGs to underspend 0.5% of their allocations to create a system reserve. This increases the resources available to spend by a further £370m. (While not increasing overall funds, the requirement to spend a further 0.5% of allocations on non-recurrent items of expenditure has also been removed.)
The £603m is being distributed on the basis of simple fair shares, in proportion to CCGs’ target allocations, which have been updated to reflect the latest population estimates.
Speaking to the NHS England board a week after the guidance was published, chief financial officer Paul Baumann said it would not have been appropriate to assign the money in a more differential way on this occasion, as all CCGs were facing current pressures. However, one CCG – South Worcestershire – has also received an additional £1.1m to ensure that it joins all other CCGs in being no more than 5% below its updated target allocation.
As part of a commitment to protect planned investment in mental health, cancer and primary care, CCGs will all be required to meet the mental health investment standard (where mental health funding grows faster than a CCG’s overall funding growth). With the centre clearly taking this issue seriously, CCG auditors will be asked to validate the achievement of this standard.
The £400m CSF mirrors the financial framework for providers and provides a targeted fund to support CCGs that would otherwise be unable to live within their means in 2018/19. All CCGs are being given control totals and any that have been set a deficit control total will be eligible for the CSF. The idea is that CSF allocations will be set at a level to enable the CCG to achieve in-year balance and will be conditional on delivery of the control total.
According to Mr Baumann, there are about 50 CCGs implementing recovery plans to eliminate structural deficits. The new fund would be used in cases where ‘even with stringent measures to close the gap’, it would take longer than one year to do so.
‘Rather than leave them to rack up ever bigger accumulated deficits – some of which are now reaching proportions that mean they have little chance of repaying them over any reasonable period – we are proposing to provide non-recurrent funding equivalent to their in-year deficit in 2018/19,’ Mr Baumann told the board meeting.
While there were obvious rewards for the CCGs concerned, the whole system would benefit. ‘The amount of national resource consumed by the most challenged CCGs will be minimised and over time there will be more money for routine allocations and drawdown of historical surpluses for CCGs that have them.’
STF rebranding
The provider sector was forecasting a £623m deficit at Q2 after taking account of use of the existing £1.8bn sustainability and transformation fund (STF). So, to meet the pledge agreed at the NHS England board in November – to ‘deal with current levels of unfunded care (deficits) that need funding going into next year’ – the STF has been increased to £2.45bn in 2018/19 and rebranded as the PSF. This also creates the headroom to remove the 0.5% system reserve requirement on CCGs, which in 2017/18 will still be needed to offset the provider overspend.
Together, the increase to the PSF and the new CSF mean an additional £1.05bn is being made available to support the costs of care currently being provided. With these funds, NHS England is clear that ‘the CCG sector is expected to achieve budget balance in 2018/19’, and NHS Improvement has specified that the trust sector will do the same.
As in the current year, 30% of the PSF will be linked to A&E performance – with providers having to achieve 90% on the four-hour wait target or beat their performance in the equivalent quarter of 2017/18, whichever is better. The remaining 70% is linked to the control total. Providers accepting their control totals will continue to be exempt from a number of agreed contractual performance sanctions, except those relating to mixed-sex accommodation, cancelled operations, healthcare-associated infections and the duty of candour.
On capital, the planning document highlights the extra £354m of public capital in 2018/19, announced in the autumn Budget. However, it added: ‘STPs and providers should not assume any capital resource above the level in the current 2018/19 operating plans unless NHS England or NHS Improvement have given written confirmation of additional resource.’
Approval of additional STP capital will be contingent on a ‘compelling estates and capital plan’. Plans will need to demonstrate value for money and savings to the STP over a reasonable payback period. STPs will also have to demonstrate they are maximising opportunities for self-funding using their own capital and receipts from land disposals and are ‘fully considering the use of private finance’.
Local payment reform
The tariff – set for two years starting from 2017/18 – remains in place, although local systems are encouraged to consider local payment reform. There is a particular push for payment systems to support advice and guidance services. Local tariffs should also be introduced for emergency ambulatory care to replace current A&E and non-elective tariffs for appropriate conditions (see Healthcare Finance, September 2017, page 23).
The allocations allow for a 1% headline pay settlement and so do not reflect any increased pressure that would arise from the government’s commitment to raise the current pay ceiling.
Growth on specialised services has increased from the previously planned 4.4% to 6.6%. The additional £354m in part reflects an updated review of new drugs likely to receive NICE approval. However, it is recognised that staying within budget will still require a substantial programme of planned efficiencies and ‘the consideration of affordability constraints’.
The planned 2018/19 allocation for general practice has been maintained but not increased further, as these commitments were seen as sufficient to cover expected cost uplifts and extended access targets set out in the General practice forward view.
The joint planning document puts a focus on system working, calling for more system-wide estates reviews and for efficiency opportunities to be looked for across organisational boundaries – for example, by reducing avoidable demand and sharing clinical support and back office functions. STPs are also expected to strengthen governance arrangements and improve engagement with communities and other partners.
It also introduces integrated care systems (ICSs) as the new name for devolved health and care systems and accountable care systems. The recent associations of the accountable care description with accountable care organisations in the US have made the term toxic and the relabelling provides an opportunity to market the new ICSs. They are described as being ‘where health and care organisations voluntarily come together to provide services for a defined population’.
There is a clear attempt to put clear water between the systems approach and any suggestion of encouraging greater private sector involvement in the health service providing whole packages of care to populations. The eight shadow ACSs – plus the two devolved health and care systems, Manchester and Surrey Heartlands – have been asked to prepare a single system operation plan narrative that encompasses CCGs and NHS providers, rather than provide individual organisation plan narratives.
This narrative should align key assumptions on income, expenditure, activity and workforce between commissioners and providers. Having a credible plan to deliver a system control total will be a condition of becoming operational. And this will be overseen by a new oversight approach by NHS England and NHS Improvement, focusing on the assurance of system plans rather than organisation-level plans.
Within ICSs, individual organisations will be able to vary their individual control totals, with agreement from the oversight bodies, as long as the system control total is met. Systems will be encouraged to adopt a system-based approach to the PSF and CSF, under which no payment is made unless the system as a whole has delivered against its system control total. If the system achieves its target but individual organisations do not, the system will still receive its sustainability funding, but NHS England and NHS Improvement will have a role in how the funds will be shared.
In return for adopting this system-wide approach, a system would enjoy a ‘more autonomous regulatory relationship’ with regulators. If an organisation within an ICS is subject to intervention, the system leaders could have a key role in agreeing what remedial action to take.
King’s Fund director of policy Richard Murray believes this could be an important new lever. ‘This holds out the possibility that where intervention is needed, ICS leads will decide what to do and the national bodies will then carry out their instructions,’ he says. ‘We must see how this new offer plays out, but it could be a game-changer in terms of ICS powers and the relationship with the centre.’
This system incentive structure will be mandatory for ICSs by 2019/20. In the meantime, systems may opt for an interim approach where only the additional funding put into the PSF (£650m in aggregate) is linked to system financial performance.
NHS Providers’ Ms Cordery says it was helpful to get further guidance on how system working is expected to develop. ‘But we would like to see a more formal and extensive engagement and consultation process on the national policy direction, along with more clarity on support for local systems which, for good reason, are finding this transition difficult,’ she said. ‘We also need realism on how fast the required transformation will occur, given how much less we are investing in change compared to the assumptions made when the Five-year forward view was created.’
Draft organisational operating plans need to be submitted by 8 March, with board-approved plans following on 30 April.
There appears to be a lot of support for the general approach. Commentators remain supportive of the push towards more integrated care and system working. And the steps towards real system incentives and system regulation are seen as good moves forward. However, there remains concern that, even with the increase in funding, there is still the underlying problem of overall resourcing for the health service.
Commissioners still face 3% efficiency targets and providers more than 4% – both in line with the current year, when it is recognised that services have been stretched to the maximum.
Ms Cordery says the extra money in the Budget has simply ‘turned an impossible task into an extremely difficult one’. Mr Dickson describes the guidance as providing a ‘set of temporary solutions’. And both bodies are united in continuing to underline the need for a new long-term funding settlement for health and social care.
Related content
We are excited to bring you a fun packed Eastern Branch Conference in 2025 over three days.
This event is for those that will benefit from an overview of costing in the NHS or those new to costing and will cover why we cost and the processes.